Bulletin # 32-16
November 14, 2016
Health Benefit Claims
Brothers and Sisters of Local 13, 63, and 94
We all acknowledge the confusion around us about how to handle our Health Insurance coverage and more importantly how to resolve demands for payment of medical bills. Be assured that your Officers are doing all we can possibly do to make these tasks easier for you and your family. However, to meet these goals we now need your help.
We need every member to be more diligent and proactive in your selection of health providers with special attention paid to whether you are selecting an “in-network” or an “out of network” provider. Also, we need your help to address recent demands from providers who are claiming members have overdue accounts for previous services by being more aware of the necessary deadlines relating to demanding payment of overdue bills, and what you must do under the requirements of the Health Plan to get those bills paid.
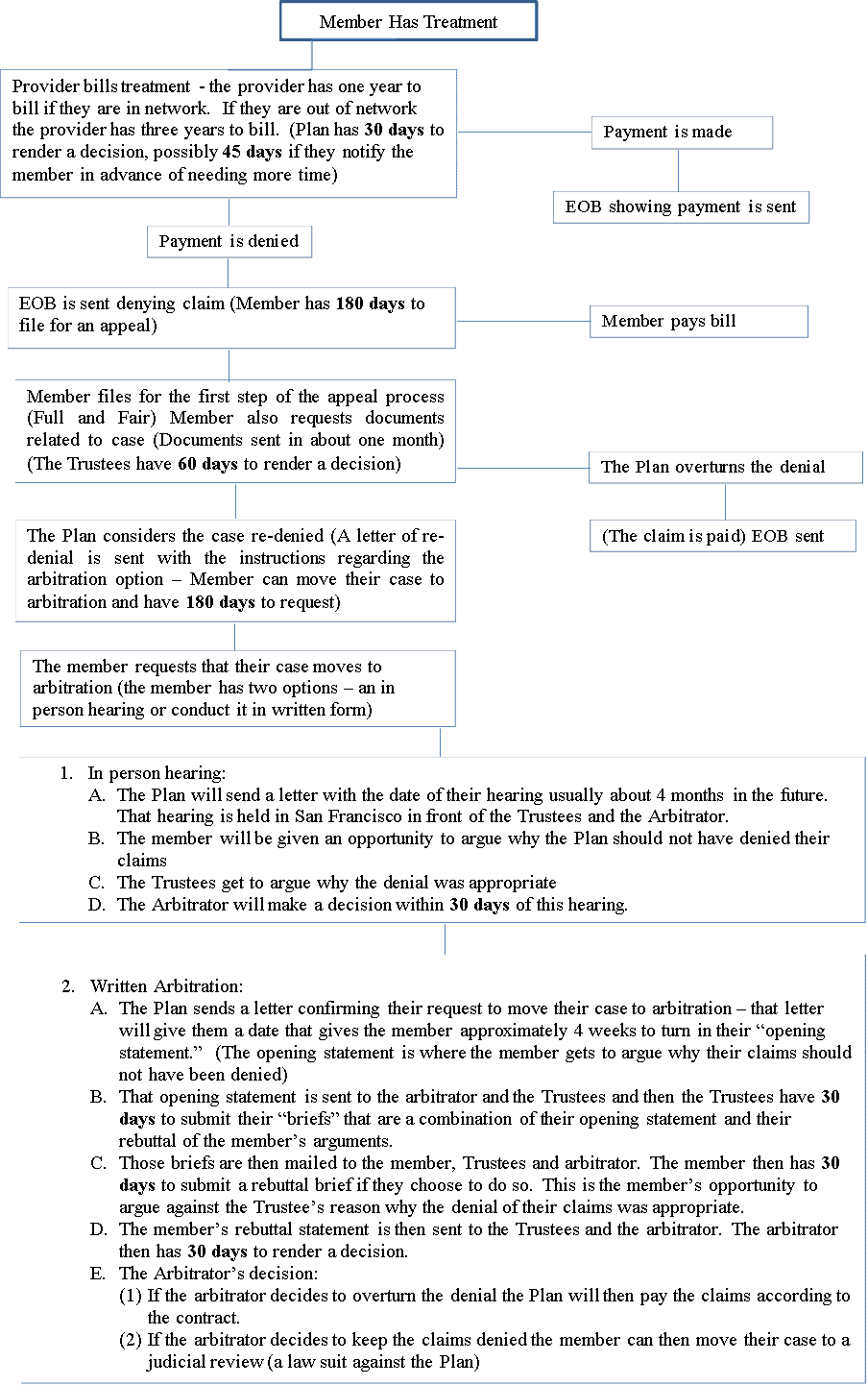
To help you become more aware of these deadlines, and how to handle those demand letters for payments, the Officers have prepared a timeline of how to handle denials of payments. This timeline graph should help you navigate the waters of the complexities of the health insurance business.
Remember, you have a right to challenge the denial of payment. That right is guaranteed by law and the Health Plan regulations and is outlined in your Supplemental Summary Plan Description (SSPD) booklet (if you do not have one please ask for one because this booklet is very important and helpful).
However, you must pursue this right or it will be lost. The attached flow chart sets forth the appeal process for each step. It also explains what you are expected to do during those steps.
As noted at the bottom, an appeal is solely and exclusively your decision and your responsibility. The only person or people that are made aware of all the documents and decisions in written correspondence is the claimant (you the member), Plan personnel, the Trustees and the Arbitrator. It is your responsibility to take note and follow your timelines.
This process is not new, but is being sought by members more often these days. Should you have questions or need assistance in starting or understanding this process beyond the enclosed document, please see your Local Officers, the Southern California Area Welfare Director, or the ILWU-PMA Benefit Plans Office (the Plan) directly.
Brothers and Sisters, you are not alone in resolving your claims, but unfortunately it takes you to initiate this process and seek the necessary assistance. Each of the locals in your area have taken the time to provide you with the tools you will need to make this process successful for you.
Please review the enclosures to familiarize yourself with the appeal process, so you can understand your rights and responsibilities. Remember to always review your Explanation(s) of Benefits (EOBs) so you will know when your claim is considered a “true denial” and you may have to file for an appeal with the Plan. This is your responsibility and has become increasingly more important.
Click for larger image